Published March 21, 2024
-
9 mins read
Integrating Patient Care Coordination with Advanced Meeting Management

Shaimaa Badawi
In the rapidly evolving landscape of healthcare, ensuring effective communication and seamless patient care coordination stands as a cornerstone for achieving optimal patient outcomes.
This article addresses the critical challenges faced by healthcare providers and explores the various aspects, benefits, importance, and use cases of care coordination. Read on to find out how care coordinators can enhance their processes by leveraging meeting management technology.
What is patient coordination?
Patient care coordination is the strategic management of healthcare services for individuals, integrating medical, psychological, and social care by enhancing communication and information sharing among healthcare professionals. This approach aims to optimize patient safety and outcomes by ensuring care activities are efficiently organized and patient information is effectively communicated across all involved parties.
Through coordinated efforts, healthcare providers aim to understand and meet patient preferences and needs, contributing to more personalized, effective, and safe healthcare delivery. This process supports smoother transitions between care settings, minimizes the risks of information silos, and promotes comprehensive care plans that address the full spectrum of a patient's needs, leading to improved health outcomes and patient satisfaction.
What's the importance of patient care coordination?
Patient care coordination is essential for streamlining healthcare delivery, enhancing safety, and improving outcomes. It reduces fragmentation in the healthcare system by ensuring seamless communication and information sharing among all healthcare providers involved in a patient's care.
This coordination prevents unnecessary tests, lowers the risk of medication errors, and avoids adverse health events. It leads to more personalized and effective care for patients, particularly those with chronic conditions or complex needs, by aligning treatment plans with their health goals. For healthcare providers and payers, it means more efficient care processes and reduced costs from avoiding unnecessary services. Ultimately, care coordination is key to a patient-centered, efficient, and effective healthcare system.
What does the care coordinator do?
A care coordinator serves as the pivotal link between patients and their healthcare teams, ensuring that all aspects of a patient's healthcare journey are seamlessly managed. This role involves conducting initial assessments to identify a patient's healthcare needs, preferences, financial resources, and support network. Based on this assessment, the care coordinator outlines potential services and options through a detailed report, helping to navigate the complex healthcare landscape.
The responsibilities of a care coordinator extend to arranging services, providing information on managing healthcare expenses, applying for benefits, and facilitating access to required medical services. They offer both ongoing support and periodic check-ups to adapt to changing conditions or needs, ensuring that patients receive continuous, high-quality care. This includes maintaining open communication lines with all parties involved, educating patients and their families about healthcare options and treatments, and coordinating case management tasks like paperwork and referrals to specialists.
When should care coordination be applied?
Care coordination becomes crucial in a variety of situations to ensure patients receive comprehensive, seamless, and personalized healthcare tailored to their unique needs and circumstances. Here are some examples:
- The management of chronic illnesses like heart disease, diabetes, or cancer, where care must be synchronized across various healthcare specialists.
- The aftermath of an emergency hospital visit, ensuring that the transition to follow-up care is seamless and effective.
- Situations where patients are juggling multiple medical conditions, necessitating a careful balance of treatments to avoid conflicts.
- The treatment of traumatic injuries, which often require a holistic approach to address both physical injuries and any associated psychosocial challenges.
- The care for elderly individuals who have multifaceted medical needs and rely on an array of caregivers and support mechanisms.
- Instances requiring coordination between healthcare and social services to support a patient's broader social determinants of health, like access to food, housing, or transportation.
- The provision of care to patients with mental health conditions, necessitating coordination between mental health professionals and medical healthcare providers.
- Cases where a patient's religious beliefs play a significant role in their care decisions, ensuring treatments align with their values.
How do patients benefit from effective care coordination?
Patients experience significant advantages from well-implemented care coordination, including the following:
- Streamlined healthcare pathways: Care coordination eliminates the fragmentation within healthcare systems, ensuring a seamless experience from primary to specialist care. This creates a continuous care pathway for patients.
- Clearer referral processes: It clarifies why referrals are made from primary care to specialists, simplifying the appointment scheduling process and providing clear next steps after specialist visits.
- Enhanced communication: It acts as a crucial link between primary care providers and specialists, ensuring both parties have complete and accurate patient information. This includes sharing reasons for referrals, diagnostic tests performed, and outcomes of specialist visits.
- Avoiding patient’s data loss: By addressing the challenges faced by referral staff in managing diverse processes and information from multiple providers, care coordination helps prevent the loss of vital patient records, making care more efficient and effective.
How healthcare providers facilitate accessible care coordination
Healthcare providers employ several strategies to make care coordination accessible and efficient, enhancing patient care and health outcomes. Here are the key methods used:
1. Electronic Health Records (EHRs)
Providers utilize a unified platform for electronic health records, allowing each healthcare professional to view and update a patient's medical history. This system facilitates seamless communication through electronic apps, ensuring all team members have access to current patient information.
2. Accountable Care Organizations (ACO)
By joining an ACO, a network of doctors, hospitals, and healthcare professionals collaborates to deliver high-quality, coordinated healthcare. ACOs focus on improving patient outcomes and managing costs, often supporting enhanced communication between primary care providers and specialists and linking patients with necessary social services.
3. Participation in special programs
Healthcare providers may engage in programs such as the CMS Innovation Center model or the Medicare Shared Savings Program. These initiatives offer guidance and incentives for effective care coordination, promoting collaborative efforts among providers to improve patient health.
4. Care conferences
Providers organize care conferences to discuss a patient's treatment plan collectively. This assembly allows for shared decision-making and the establishment of a unified care plan, serving as a guide for the healthcare team's goals and actions.
5. Centralized digital patient information
The adoption of EHRs provides a centralized, digital database of patient information, accessible to all medical professionals involved in a patient's care. This ensures that each provider can make informed decisions based on the latest patient data.
6. Compliant communication methods
Care coordination is supported by secure and compliant communication channels, including email, virtual conferences, faxes, or phone calls, adhering to HIPAA regulations. Care coordinators ensure that accurate contact information is available for all team members.
7. Patient education
Educating patients and their caregivers about their condition and treatment options empowers them to actively participate in their care. Informed patients can advocate for their health effectively, making them integral members of the care coordination process.
Use case example for patient care coordination
Mrs. Thompson, 65, diagnosed with early-stage breast cancer, benefits from an exemplary care coordination approach. Upon diagnosis, her primary care physician connects her with a care coordinator, an oncology-experienced nurse, who assembles a comprehensive care team. This team includes an oncologist, surgeon, radiation therapist, mental health counselor, and nutritionist, ensuring a holistic approach to her treatment and well-being.
The coordinator also facilitates home health assistance and physical therapy to support Mrs. Thompson’s daily needs and physical health. Regularly scheduled care conferences and the use of telehealth services reduce Mrs. Thompson's travel burden and keep her treatment responsive and well-managed.
The use of a shared electronic health record system ensures all team members have access to up-to-date information about her treatment and responses. This coordinated care model ensures Mrs. Thompson receives seamless, multidisciplinary support throughout her treatment journey, aiming for the best possible health outcomes and quality of life.
What are the challenges of patient care coordination?
The complexities of healthcare communication and coordination present several challenges for professionals aiming to deliver value-based, efficient patient care:
1. Outdated communication channels: Healthcare teams often depend on older methods like faxing for communication, causing delays in urgent care situations.
2. Test result delays: Unlike the real-time tracking available for deliveries, many healthcare settings lack immediate monitoring of patient test results, leading to long waits and impacting care planning.
3. Data security concerns: The healthcare industry faces significant risks with data security, including the mishandling of records and vulnerability to ransomware attacks, jeopardizing patient confidentiality and leading to financial losses.
4. Adapting to rapidly changing security standards: Healthcare providers struggle to keep up with fast-evolving data security standards and compliance regulations, increasing the risk of data breaches.
5. Integration of AI and machine learning: While AI and machine learning offer opportunities to enhance care coordination through automation and efficiency, the adoption of these technologies also presents challenges in implementation and training.
How adam.ai can facilitate communication in patient care
Transitioning from the outlined challenges in care coordination communication, it becomes evident that healthcare providers are in dire need of a streamlined, secure, and efficient solution to navigate these complexities. This is where a meeting management product, like adam.ai, steps into the picture. Designed with the specific needs of healthcare professionals in mind, this innovative platform revolutionizes care coordination by addressing each of the aforementioned pain points head-on.
Here's what you can do with adam.ai:
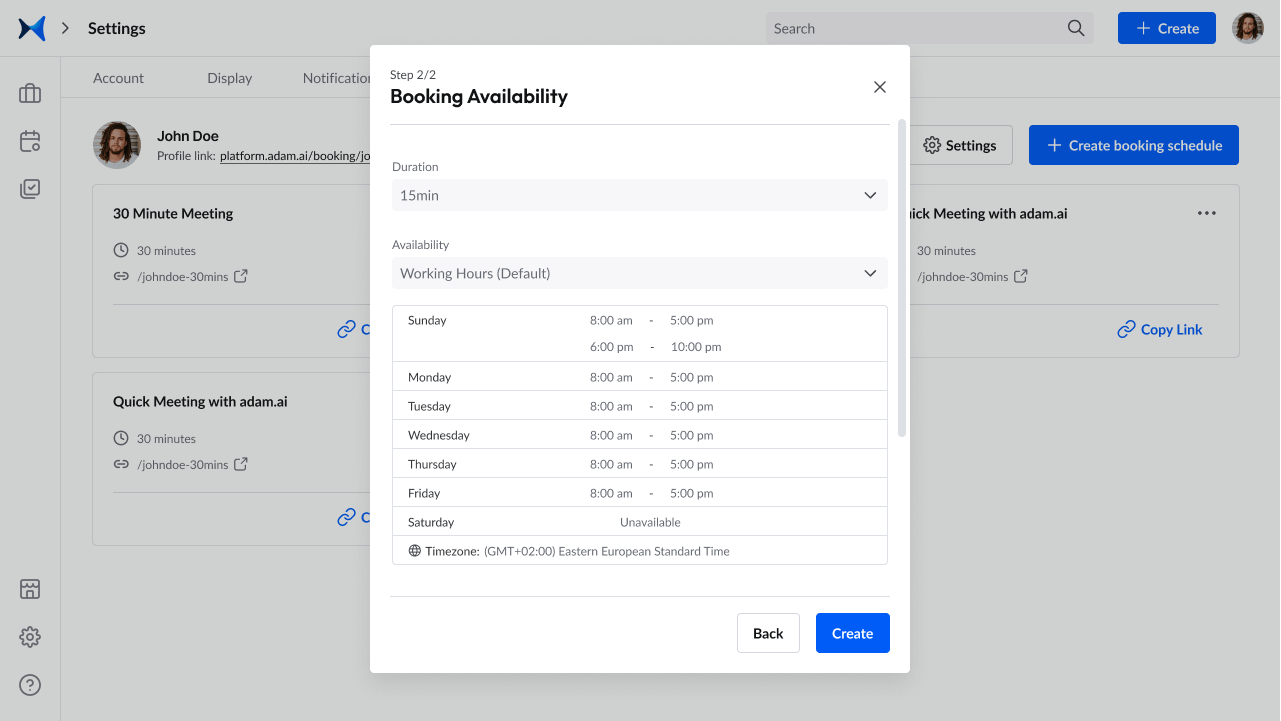
1. Create unlimited booking pages to streamline the process of organizing meetings between different stakeholders in a patient's care, including specialists, primary care providers, and even family members.
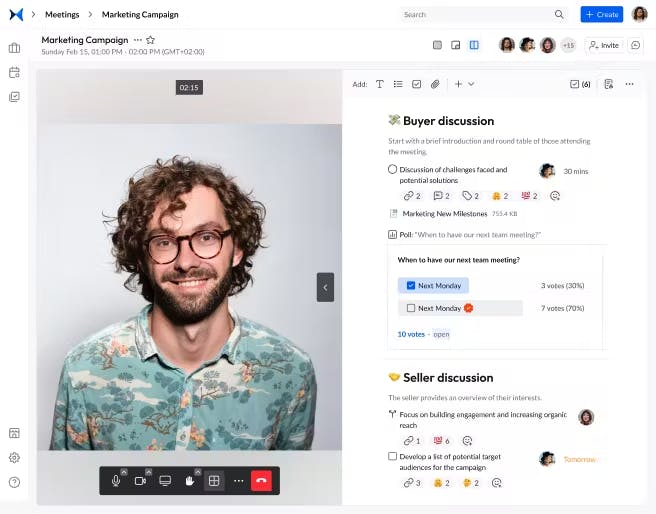
2. Record agenda items, actions, polls, decisions, and notes using a smart note-taking system displayed side by side with the built-in video-conferencing feature to discuss patient care plans, share updates, and make decisions without the delays that come from scheduling in-person meetings.
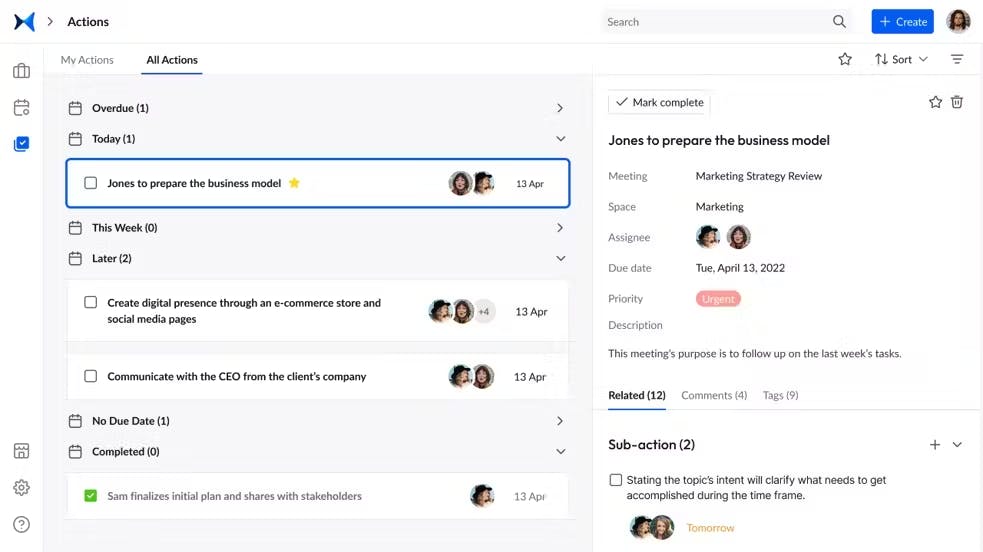
3. Track your actions and decisions for patient care plans and follow-up schedules to never miss an update on the patient's health condition and medical history.
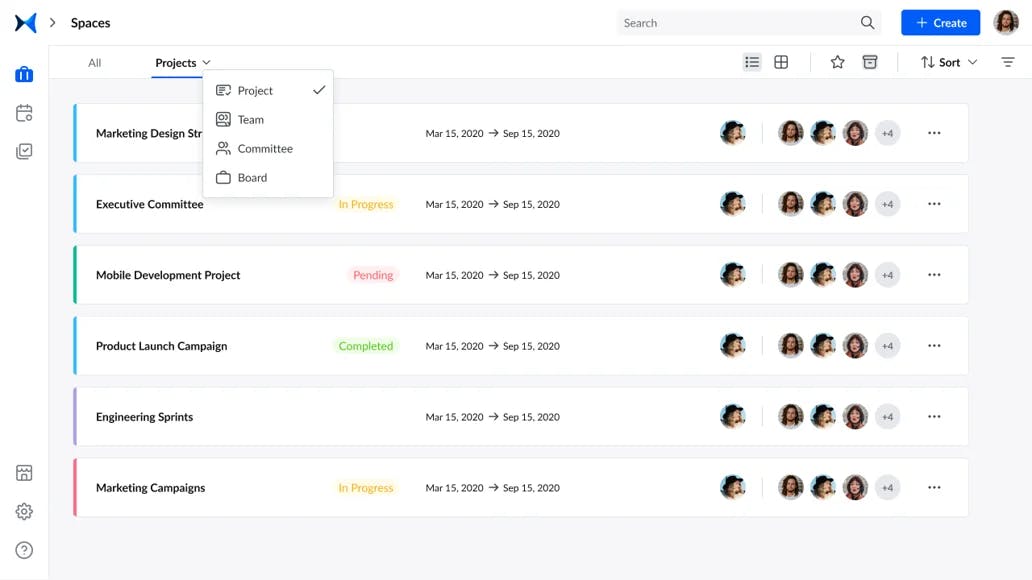
4. Categorize meetings into spaces to include different healthcare personnel under the teams or projects category to keep records of the patient's medical history under a specific umbrella.
5. Generate and share meeting minutes for due diligence and to keep the patient's record for future reference.

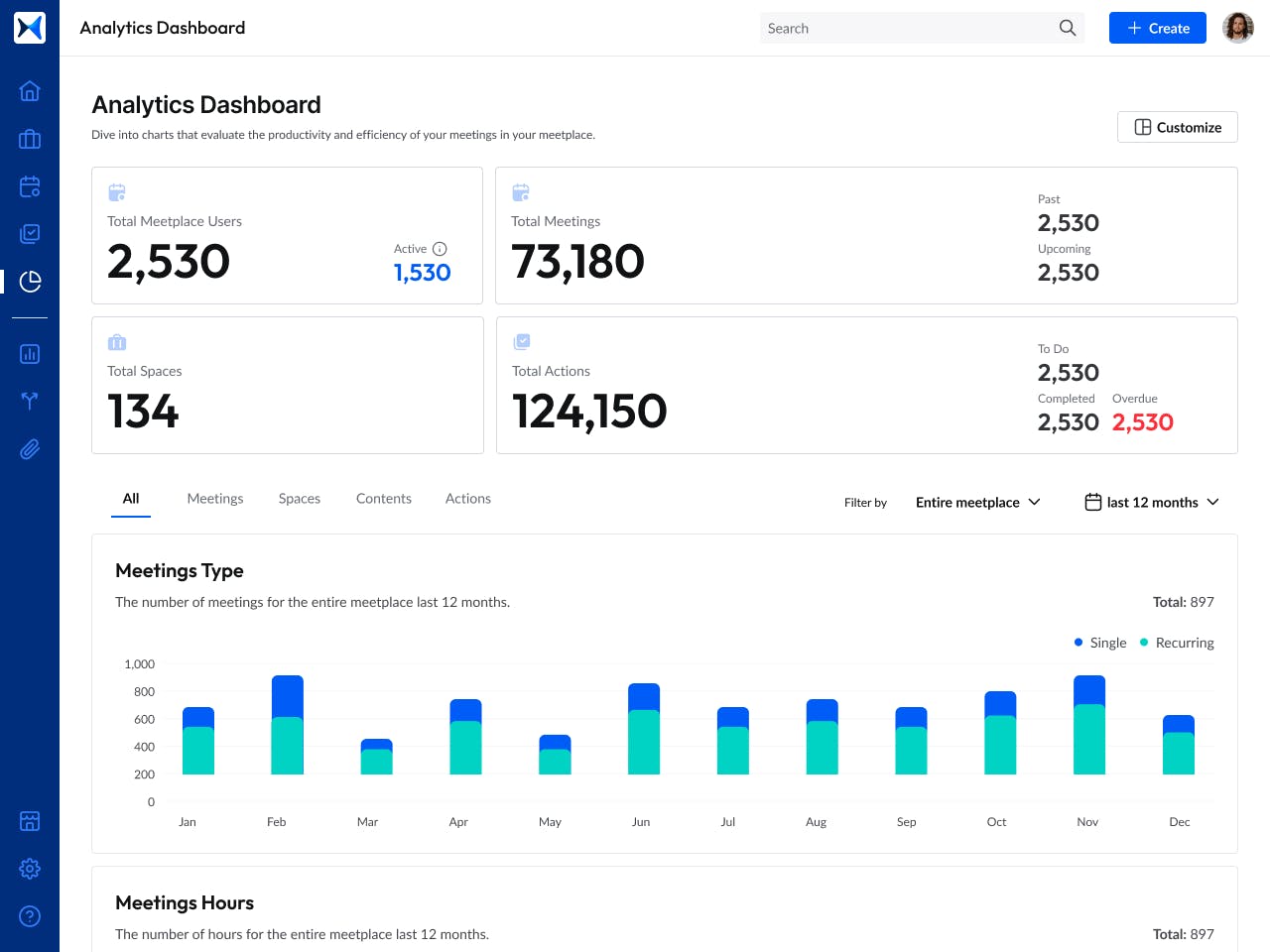
6. View the analytics dashboard to evaluate participation rates, decision outcomes, and the progress of action items to facilitate smooth and effective meetings and integrate seamlessly with the healthcare ecosystem
All patient information is kept on a secure platform with all actions, decisions, agenda items, and uploaded files to facilitate the requirements of patient care coordination and streamline the process for healthcare providers and care coordinators.
Get started right now to streamline communication and coordination of patient care.
The bottom line
Addressing the challenges of patient care coordination is critical in enhancing the effectiveness, safety, and efficiency of patient care. As healthcare professionals navigate these obstacles, the potential for improvement in patient outcomes and system efficiency is immense.
By focusing on innovative approaches and technologies to streamline communication and coordination, the healthcare industry can move towards a more integrated and patient-focused care model.
And while there may be multiple meeting management solutions available, here is why adam.ai is the all-in-one meeting management platform you can trust:
- adam.ai is one of Atlassian Ventures' portfolio companies.
- In the meeting management software category on G2, adam.ai has been ranked a leader and a high performer for successive quarters in the past years.
- adam.ai has been included in the Forrester Report in the AI-enabled meeting technology landscape.
- adam.ai is trusted and used by powerful teams and organizations worldwide for all types of critical meetings, like board, committee, project management, and business development meetings.
- And most importantly, adam.ai integrates with your existing workflow, is SOC2 compliant, provides dedicated support and success, and has a free trial option.
About the author ...
Shaimaa Badawi is an Inbound Marketing Specialist at adam.ai. Her research revolves around meeting management, project management, and board meetings, where she identifies the most daunting meeting pain points that C-level executives, board and committee members, corporate secretaries, and other professionals working in enterprises face in meetings. Based on her findings, Shaimaa provides solutions for inefficient meetings, defines various aspects of corporate-level meetings, and outlines best practices on how to run effective meetings.
Subscribe to our blog
Subscribe to our blog
Get the latest blog posts sent straight to your inbox.


